When we go to the hospital, we often have to wait at different places. Nurses are busy with computers or walking around. Receptionists spend a long time typing in information. And doctors spend more time looking at computers than talking to us.
Well , reality is Healthcare Efficiency often takes a backseat to the system designed around staff convenience, bureaucracy and administrative needs – unfortunately not around patients.
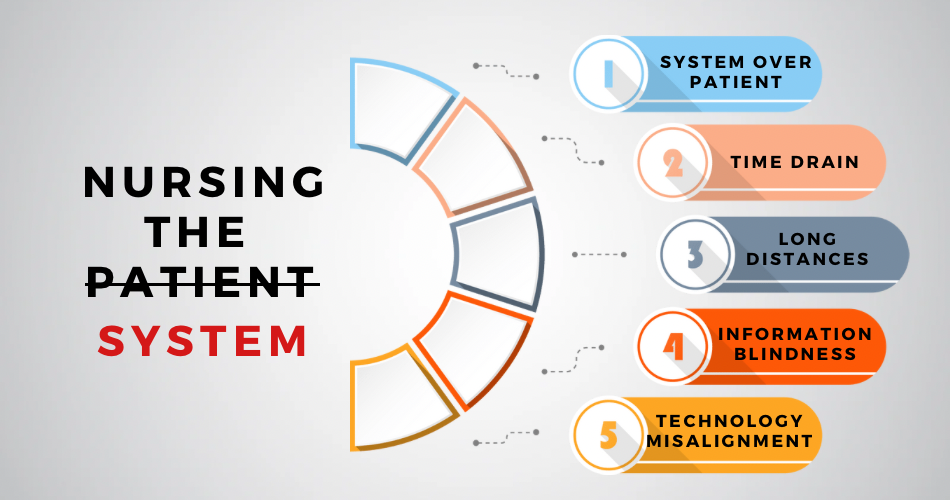
System over Patient
Hospitals are often structured around the needs of the institution and its staff rather than the well-being of patients. This systemic approach leads to a disconnect between the delivery of care and the actual needs and preferences of patients.
- One-Size-Fits-All Approach: Standardized procedures and protocols, while necessary to some extent, can overlook the individualized needs of patients, resulting in a less personalized and potentially less effective care experience.
- Resource Allocation Challenges: Budgetary constraints and administrative priorities may dictate resource allocation decisions, sometimes at the expense of optimal patient care delivery.
- Inflexible Processes: Rigid workflows and bureaucratic red tape can hinder nimble responses to patient needs and emergent situations, contributing to delays and frustrations for both patients and healthcare providers.
Time Drain – Nurses and other healthcare workers, with their unwavering dedication to patient care, often find themselves grappling with an overwhelming amount of administrative tasks and procedural hurdles that consume valuable time.
- Administrative Overload: From updating patient records to coordinating with various departments, nurses spend a significant portion of their shifts on paperwork and bureaucratic tasks, detracting from direct patient care interactions.
- Resource Scarcity: Limited access to essential materials, equipment, and information further compounds the time drain, forcing nurses to spend precious minutes searching for supplies or navigating convoluted systems to retrieve critical data.
- Workflow Interruptions: Constant interruptions, whether it’s responding to calls, attending meetings, or addressing emergent issues, disrupt the flow of patient care activities, fragmenting nurses’ time and attention.
Long Distances – Within the labyrinthine corridors of hospitals, nurses often find themselves traversing significant distances to fulfill their duties, contributing to a substantial loss of time and energy.
- Physical Strain: Constantly navigating sprawling hospital campuses and multiple floors can take a toll on nurses’ physical well-being, leading to fatigue and decreased productivity.
- Time Consumption: The minutes spent traversing long distances between patient rooms, supply closets, medication dispensing stations, and administrative offices add up, detracting from valuable face-to-face interactions with patients.
- Delayed Responses: Lengthy travel times between locations within the hospital can lead to delays in responding to patient needs, potentially compromising the timeliness and quality of care delivery.
Information Blindness – Despite the wealth of data generated within healthcare systems, nurses often find themselves grappling with information overload or, conversely, facing critical gaps in access to essential patient data.
- Data Overload: Nurses may be inundated with an overwhelming amount of data from electronic health records (EHRs), diagnostic tests, medication orders, and care plans, making it challenging to distill relevant information and make timely decisions.
- Fragmented Systems: Disparate information systems and siloed data repositories can result in fragmented patient records, inhibiting comprehensive assessment, coordination of care, and continuity across different healthcare settings.
- Lack of Context: Without contextual information about a patient’s medical history, treatment preferences, and social determinants of health, nurses may struggle to provide holistic, patient-centered care tailored to individual needs.
Technology Misalignment – Despite the promise of technological advancements to revolutionize healthcare delivery, many healthcare systems struggle with a pervasive misalignment between technology solutions and the needs of frontline providers and patients.
- Legacy Systems: Outdated legacy systems and software platforms may lack interoperability, usability, and functionality, hindering seamless information exchange and workflow integration.
- User Experience Challenges: Clunky interfaces, cumbersome workflows, and poor usability design contribute to user frustration and resistance to adopting technology solutions, impeding the realization of their potential benefits.
- Workflow Disruption: Poorly integrated or poorly implemented technology solutions can disrupt established workflows, leading to inefficiencies, errors, and resistance to change among frontline staff.
Harnessing Lean Thinking for Transformation:
Value-Added Analysis: Conduct a thorough examination of workflows to identify and eliminate non-value-added activities, ensuring that every action contributes directly to improving patient outcomes and experiences.
Patient-Centered Design: Place patients at the heart of process design, involving them in decision-making and tailoring care plans to their individual needs, preferences, and circumstances.
Patient Engagement: Empower patients to actively participate in their care by providing access to their health information, encouraging shared decision-making, and fostering partnerships between patients, families, and healthcare
Gemba Walks : Get leadership involved at the frontline to understand challenges firsthand and drive meaningful change.
Spatial Optimization: Utilize principles of lean facility design to optimize the layout of hospital units, supply storage areas, and workstations, minimizing the need for excessive travel and reducing time spent navigating the physical environment.
Mobile Workstations: Implement mobile technology solutions and portable workstations that enable nurses to access essential information, document care activities, and communicate with colleagues without being tethered to stationary computers or desks.
Task Bundling: Strategically bundle tasks and activities to minimize the number of trips nurses need to make between different locations within the hospital, maximizing efficiency and reducing unnecessary movement.
Just-in-Time Delivery: Adopt just-in-time inventory management practices to ensure that supplies and equipment are replenished precisely when and where they’re needed, minimizing the need for nurses to travel to distant storage areas to travel to distant storage areas to retrieve items.
Visual Management: Visual cues and organized workstations can optimize efficiency, minimizing time spent searching for materials and information.
Standardization Procedures : Establishing standardized procedures ensures consistency and eliminates unnecessary steps, allowing nurses to focus on patient care.
Empowered Frontline Staff: Cultivate a culture of empowerment and accountability. Equip nurses and other frontline healthcare providers with the autonomy and resources to advocate for their patients and innovate solutions that prioritize patient well-being.
Data Driven Insights : Leverage data analytics to identify patterns, trends, and areas for improvement, empowering healthcare teams to make informed decisions.
Optimized Resource Allocation: Utilize data-driven insights to identify resource utilization patterns and optimize inventory management systems, ensuring that essential materials and information are readily accessible when and where they’re needed.
Continuous Feedback Loops: Implement mechanisms for soliciting and incorporating feedback from patients, caregivers, and frontline staff into ongoing process improvement efforts, ensuring that the system remains responsive and adaptive to evolving needs and challenges.
Continuous Improvement: Embracing a culture of continuous improvement encourages feedback and innovation, driving ongoing enhancements to patient – focuses practices.
Hospitals should overhaul the outdated systems and put patients back at the center of healthcare delivery where efficiency and compassion go hand in hand.