A hospital command center is a centralized hub that enables real-time, data-driven decision-making to optimize patient care, streamline operations, and improve overall efficiency in a healthcare setting. It involves the use of advanced technology, analytics, and process engineering to coordinate and manage patient flow, bed management, staffing, and other critical functions. By bringing together cross-functional teams and providing them with accurate, up-to-date data, it empowers healthcare professionals to make better decisions, faster.
It is also known as a capacity command center, and can greatly enhance a healthcare organization’s ability to respond to changing conditions, anticipate potential issues, and ensure optimal patient outcomes.
The concept of a command center is not new; it has been successfully applied in other industries, such as aviation, supply chain management, and emergency response. However, the healthcare industry has only recently begun to adopt this approach to address the growing challenges of patient care, resource management, and financial pressures. As hospitals continue to face increasing demands, the need for innovative solutions like a hospital command center becomes more important than ever.
The recent global pandemic has highlighted the importance of hospital command centers in managing healthcare services during a crisis. As Matt Metsker, division director for mission control and virtual health services at Virginia Mason Franciscan Health in Washington state, stated in a HealthTech article, the command center enabled the organization to make real-time data-driven decisions and quickly adapt to changing circumstances. The pandemic has further emphasized the need for efficient command centers in healthcare organizations.
Benefits of implementing a hospital command center
Implementing a hospital command center can provide numerous benefits for healthcare organizations. These benefits can lead to improved patient outcomes, increased efficiency, and more effective use of resources.
Enhanced Patient Care
A hospital command center enables healthcare providers to monitor patient conditions, treatment progress, and resource availability in real time. This allows healthcare providers to make more informed decisions about patient care, leading to better outcomes and increased patient satisfaction.
Streamlined Operations
By centralizing critical functions and providing a single source of truth, it can help hospital staff identify bottlenecks, prioritize tasks, and allocate resources more effectively. This can lead to reduced wait times, faster patient throughput, and more efficient use of hospital resources.
Improved Communication, Collaboration, and breaking down silos
A hospital command center brings together cross-functional teams, fostering communication and collaboration among healthcare professionals. This can lead to more informed decision-making and a more coordinated approach to patient care, ultimately improving the patient experience.
Combating Clinician Burnout
By incorporating remote solutions, hospital command centers can help combat clinician burnout. As an example, the integration of a virtual nursing program could enable nurses who are stretched thin to alternate their presence on the floor and provide remote assistance to newer nurses at the bedside. This not only benefits newer nurses by giving them access to experienced support but also improves work-life balance for older nurses, leading to higher employee satisfaction and improved clinical outcomes.
Cost Savings
By optimizing resource utilization and reducing inefficiencies, a hospital command center can help healthcare organizations save money. These cost savings can be reinvested in patient care, allowing hospitals to offer more services and improve overall patient outcomes.
Key components
An effective hospital command center is built on several key components that work together to optimize hospital operations and improve patient care.
Advanced Technology
A hospital command center relies on advanced technology to collect, analyze, and display real-time data from various sources, such as electronic health records (EHR), patient monitoring systems, and hospital information systems. This technology enables healthcare professionals to make data-driven decisions and respond quickly to changing conditions.
Data Analytics
Effective data analytics is crucial for hospital command centers to make informed decisions. By analyzing real-time data from various sources, command centers can identify trends, predict patient needs, and allocate resources efficiently.
Cross-Functional Teams
An effective command center brings together cross-functional teams, such as clinical staff, administrators, and support staff, to collaborate and make decisions based on real-time data. This collaborative approach helps to ensure that all stakeholders are working together to optimize patient care and hospital operations.
Remote Monitoring
Remote monitoring allows healthcare professionals to track patient health and progress, even when they are not within hospital walls. This technology plays a crucial role in enabling command centers to support the continuum of patient care.
Process Engineering
An effective hospital command center requires a thorough understanding of the hospital’s existing processes, as well as the ability to identify areas for improvement. Process engineering techniques, such as Lean, Six Sigma, and process mapping, can help healthcare organizations identify inefficiencies and develop strategies to streamline operations.
Continuous Improvement
A hospital command center should be continually evolving and adapting to changing conditions and needs. This requires ongoing monitoring, analysis, and improvement efforts to ensure that the command center remains effective and efficient over time.’
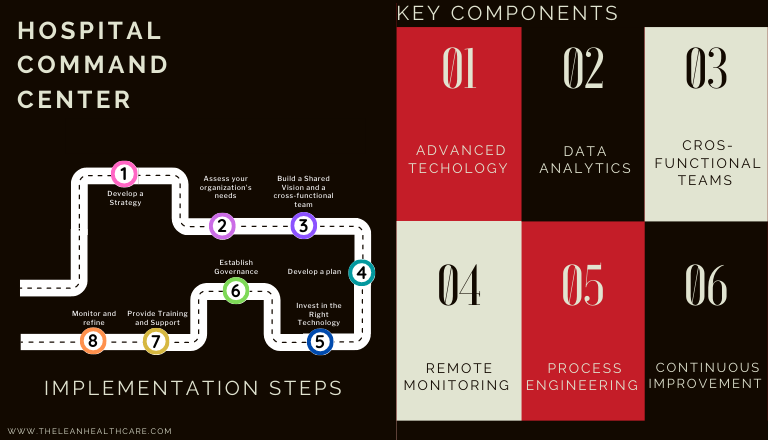
Steps to Implement a hospital command center
Implementing a hospital command center can be a complex process, but breaking it down into manageable steps can help ensure a successful outcome.
Step 1: Develop a Strategy
Before setting up a command center, healthcare organizations must establish a clear strategy that outlines their goals, objectives, and desired outcomes. This strategy should align with the organization’s overall vision and mission.
Step 2: Assess your organization’s needs
Conduct a thorough assessment of your hospital’s current processes, resources, and capabilities to identify areas where a command center could have the greatest impact.
Step 3: Build a Shared Vision and a cross-functional team
A shared vision is essential for the success of a hospital command center. All stakeholders, including care teams, administrators, and support staff, should be involved in the planning process to ensure that everyone understands the purpose and benefits of the command center.
Assemble a team of key stakeholders and this team will be responsible for developing the command center’s goals, objectives, and strategies.
Step 4: Develop a plan
Create a detailed plan outlining the steps required to implement the hospital command center, including the necessary technology, resources, and training. This plan should also include specific timelines, milestones, and performance metrics to track progress and measure success.
Step 5: Invest in the Right Technology
Selecting the right technology is critical for the success of a hospital command center. Select and implement the technology that will form the backbone of your hospital command center, such as data analytics tools, electronic health records (EHR), and patient monitoring systems. Ensure that these systems are properly integrated and that staff receive appropriate training.
Step 6: Establish Governance
Develop clear processes and protocols for using the hospital command center, including outlining how to collect, analyze, and share data, as well as how to make decisions. Ensure thorough documentation and consistent adherence to these processes to uphold the integrity of the command center.
Step 7: Provide Training and Support
Staff members must be trained and supported in using the command center effectively. This includes understanding the technology, processes, and best practices associated with the command center.
Step 8: Monitor and refine
Once the hospital command center is operational, continually monitor its performance and make adjustments as needed. This may involve refining processes, updating technology, or addressing new challenges as they arise.
Challenges and Solutions
Establishing a hospital command center can present several challenges, but with careful planning and collaboration, these challenges can be effectively addressed.
Resistance to change
Implementing a hospital command center requires significant changes to existing processes and workflows, which can be met with resistance from staff.
Solution: Engage staff in the planning and implementation process, and clearly communicate the benefits of the command center. Provide ongoing training and support to help staff adapt to the new processes and technology.
Integration of technology
Integrating new technology with existing systems can be complex and time-consuming.
Solution: Work closely with technology vendors and IT staff to ensure seamless integration and compatibility. Develop a phased implementation plan to minimize disruptions to existing workflows.
Maintaining data privacy and security
A hospital command center relies on collecting and analyzing sensitive patient data, requiring us to protect patient privacy and comply with regulations.
Solution: Implement robust data security measures, such as encryption and access controls, to safeguard patient information. Regularly review and update these measures to stay ahead of emerging threats.
Success stories: Hospital command centers in action
Healthcare organizations across the globe have successfully implemented hospital command centers, showcasing their potential to enhance efficiency and patient care.
Johns Hopkins Hospital – Baltimore, Maryland
Johns Hopkins Hospital implemented a hospital command center to improve patient flow and resource utilization. The command center has significantly reduced patient wait times, increased bed availability, and improved overall patient satisfaction.
Humber River Hospital – Toronto, Canada
Humber River Hospital’s command center helped them improve patient flow, reduce wait times, and optimize bed management by centralizing decision-making and leveraging real-time data.
Children’s National Hospital in Washington D.C.
Earlier this year, Children’s National Hospital in Washington D.C. established a telehealth command center with the aim of enhancing the monitoring of patients suffering from critical heart disease.
Duke University Health System
Duke University Health System uses its Care Hub Command Center to manage capacity and throughput across its facilities. This has enabled the health system to optimize patient flow, reduce wait times, and improve overall efficiency.
Atrium Health
Atrium Health’s virtual nursing observation program, integrated with its command center, has helped mitigate clinician burnout by allowing overextended nurses to remotely support newer staff members. This has led to improvements in employee satisfaction and clinical outcomes.
The Future of hospital command centers: Trends and Predictions
As technology continues to advance and the healthcare landscape evolves, hospital command centers are ready to take on an even more crucial role in optimizing hospital operations and patient care.
Artificial intelligence and machine learning
The integration of artificial intelligence (AI) and machine learning into hospital command centers will enable even more sophisticated data analysis and decision-making. These technologies can help predict patient needs, identify potential bottlenecks, and optimize resource allocation.
Integration with Virtual Care
The rise of virtual care services presents new opportunities for hospital command centers. By integrating with telehealth platforms and remote monitoring systems, command centers can support a wider range of healthcare services and expand their reach beyond hospital walls.
Increased focus on patient experience
As the healthcare industry increasingly prioritizes patient experience, these centers will play a key role in ensuring that patient needs are met quickly and efficiently. By streamlining operations and improving communication, command centers can help create a more patient-centered care environment.
Conclusion: The impact of hospital command centers on healthcare efficiency
The implementation of a hospital command center has the potential to revolutionize the way healthcare organizations operate and deliver care. Centralizing decision-making, leveraging real-time data, and fostering collaboration among cross-functional teams, can help optimize workflow, improve efficiency, and ultimately enhance patient care.
As technology continues to advance and the healthcare landscape evolves, the role of hospital command centers will only become more important in meeting the demands of today’s complex healthcare environment.
