Imagine a hospital where:
- Nurses spend 30% less time hunting for supplies.
- Doctors aren’t drowning in clicks instead of patient care.
- Every admin process exists to serve—not slow down—the people saving lives.
This isn’t a utopian fantasy. It’s what happens when we flip the pyramid—and Lean Thinking shows us how.
❌ The Problem: Healthcare’s Backwards Hierarchy
Every moment of healing, reassurance, or recovery happens in a direct interaction between a patient and a caregiver. Physicians, nurses, and patient admin teams are the value creators in our healthcare system.
Everything else—logistics, HR, IT, finance, and leadership—exists to support that interaction.
Yet far too often, frontline teams are overburdened by inefficient systems, disconnected processes, and administrative overhead. Instead of being supported, they’re fighting upstream to deliver care.
This isn’t just frustrating—it’s waste.
Most hospitals operate like a top-heavy pyramid:
- Top: Executives, support functions
- Middle: Managers, coordinators
- Bottom: Doctors, nurses, aides—the people actually touching patients
But here’s the irony:
- The real value—the healing, the care, the human connection—happens at the bottom.
- Yet, frontline teams waste hours daily fighting broken systems, redundant processes, and misaligned priorities.
Lean Thinking, originally developed in manufacturing but deeply applicable to healthcare, gives us a clear blueprint:
“Value is defined by the customer. Everything else is waste.”
In healthcare, the customer is the patient—and the frontline is the only team delivering that value. So why do we treat them like an afterthought?
🔄 The Lean Fix: Flip the Pyramid
Lean Thinking gives us a blueprint for redesigning healthcare around value:
1️⃣ Value = What the Patient Needs / Defined from the patient’s perspective.
- Example: A patient undergoing surgery values accurate information, pain relief, and a smooth recovery—not paperwork delays, unnecessary tests, or long waits. If a process doesn’t improve patient outcomes or experience, it may not be adding value.
- 📌 Key Action: Ask, “Does this activity improve the patient’s experience or outcome?”
2️⃣ Value Stream = This principle involves identifying and visualizing every step involved in delivering care—from admission to discharge—and identifying what adds value and what doesn’t.
- Example: Mapping the discharge process reveals 27 steps, including redundant documentation, multiple approvals, and waiting for transportation. Many of these steps delay discharge and create no value for the patient or staff.
- 📌 Key Action: Eliminate the unnecessary; streamline the necessary. Use a value stream map to expose hidden inefficiencies.
3️⃣ Create Flow = Enable Smooth, Uninterrupted Care Delivery
- Example: A nurse spending 20 minutes searching for IV pumps, supplies, or patient charts breaks the flow of care. Centralizing equipment, using visual management, or employing mobile supply carts can restore flow.
- 📌 Key Action: Ensure everything needed for care is available at the point of use.
4️⃣ Establish Pull – Provide Services Based on Real-Time Needd
- Example : Rather than stocking all wards with supplies “just in case,” implement a Kanban-based system where restocking only occurs when bins are low. In the OR, instruments are prepared based on scheduled surgeries.
- 📌 Key Action: Let the frontline “pull” what they need when they need it.
5️⃣ Pursue Perfection – Continuous Improvement Through Everyone
- Example: A frontline team runs daily huddles to surface patient flow delays, safety concerns, or equipment issues. A suggestion board invites improvement ideas from any staff member, and leaders respond quickly..
- 📌 Key Action: Make improvement part of the daily rhythm—led by those who do the work..
🏥 The Patient-Centered Hospital: A New Visual
Forget the old pyramid. Here’s the Lean-driven support structure:
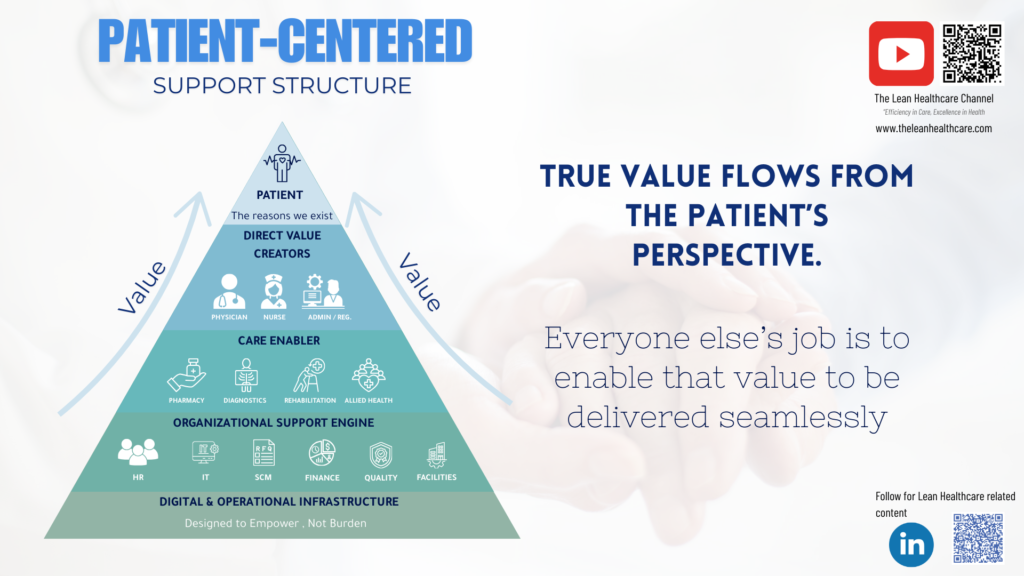
🔝 Patient – At the top: the purpose of the system
👩 Frontline Teams (Doctors, nurses, aides—the real value creators)
🛠️ Care Enablers (Pharmacy, labs, rehab—speed up, don’t slow down)
📊 Support Functions (HR, IT, finance—silent engines, not bureaucracy)
⚙️ Digital & Infrastructure (Tools should help, not hinder)
This is not just a design change—it’s a cultural one. One where we ask daily:
“What do our frontline teams need from us to deliver better, safer, faster care?”
💡 The Result: What Changes When We Flip the Script?
- Patients receive more timely, coordinated care
- Staff feel valued, empowered, and less burnt out
- Resources flow toward where they are needed most
- Continuous improvement becomes the norm, not the exception
“Lean isn’t about cutting—it’s about empowering those who matter most.”
🔴 A Call to Action (No More Lip Service)
Healthcare doesn’t need another “efficiency initiative.” It needs a reckoning:
- Leaders: Are you measuring support—or just output?
- Frontline: What’s one change that would free up 2 hours/day?
- All of us: Stop calling them “support staff.” They’re the mission control.
Let’s stop asking heroes to climb broken ladders. Build them a rocket instead.