In July 2006, 49-year-old Beatrice Vance arrived at the busy ED of Vista Medical Center East in Waukegan, Illinois, complaining of nausea, shortness of breath, and chest pain. Triaged and sent to the ED waiting room, Mrs. Vance waited there for two hours without further attention. When she was finally called, she failed to respond and was found dead of an acute myocardial infarction.
The coroner Jury found that the woman had presented with “classic symptoms of a heart attack.” The coroner’s jury ruled the death a homicide, which could lead to criminal prosecution. The coroner stated that the length of wait within the emergency room was a contributing factor in her death because she died of congestive heart failure. The piece rightly highlights the serious consequences that may occur if a triage nurse makes an error, and it also links the apparent problem here to ED overcrowding.
https://abcnews.go.com/GMA/Health/story?id=2454685&page=1=
ED Crowding
Emergency Department Crowding is a pressing issue within the healthcare sector. It’s a complex problem characterized by an imbalance between patient demand and the emergency department’s capacity to deliver quality care.
Emergency department overcrowding refers to the situation where ED function is impeded because the number of patients exceeds either the physical and/or staffing capacity of the ED, whether they are waiting to be seen, undergoing assessment and treatment, or waiting for departure.
Australasian College for Emergency Medicine
Standard Terminology for Emergency Departments
May 2023 Policy (P02) v7
ED crowding can not only compromise patient care but also result in delays in treatment, increased patient discomfort, and possible deterioration of conditions.
As overcrowding is caused by a mismatch between supply and demand, one might think that an increase in supply (hospital beds and staff) could easily solve the problem. However, a problem that appears simple does not always have a simple solution. It requires a comprehensive understanding of the healthcare system’s intricacies, the flow of patients, and the factors contributing to overcrowding.
ED crowding is not just about numbers, but about the health and well being of individuals seeking emergency care. It’s about the nurses, doctors, and staff who strive to provide the best care possible in chaotic and stressful conditions. Therefore, fully grasping the scope and implications of ED crowding is an essential first step towards resolving it.
Emergency Department Crowding – Factors
Crowding in the emergency department is often a result of a multitude of factors. It is not merely a question of too many patients, but also issues with how patients are managed within the system. It’s a multifaceted problem that cannot be solved by merely increasing capacity.
ED crowding is a systemic issue. It involves not only the emergency department but also other departments within the hospital. For instance, a backlog in the admission of patients from the ER to other hospital departments can contribute to ED crowding.
Moreover, external factors such as seasonal flu, a pandemic etc. can significantly increase the demand for emergency and choke ED. Therefore, a broad perspective is required to truly understand and address this issue.
The Issue of ER Waiting Times
One of the most evident implications of ED crowding is the issue of ER Waiting times. ER waiting times can also result in diminished patient experience.
Extended wait times and decreased patient satisfaction are just the tip of the iceberg when it comes to the effects of ED crowding. It’s not just about an overcrowded waiting room, but it’s also about the quality of care that gets compromised. When the ED is overcrowded, it strains the healthcare providers and resources, leading to potential delays in diagnosis and treatment, which could have serious repercussions on patients’ health outcomes like the case we mentioned at the beginning of the article.
Long ER waiting times can also lead to ambulance diversion, where ambulances are directed to other hospitals due to the overcrowded state of the emergency department, which can lead to delays in the provision of emergency care.
Furthermore, ER crowding and long waiting times can increase stress for healthcare providers, leading to burnout and decreased job satisfaction. This can result in a decline in staff morale, further compromising the quality of care provided.
Understanding the Causes of Emergency Department Crowding
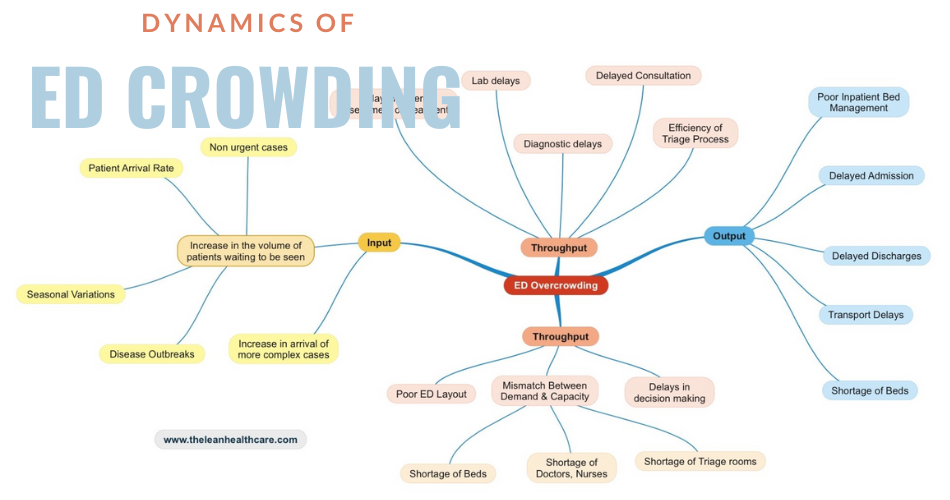
The causes of ED crowding are multi factorial and complex. They can be broadly categorized into input, throughput, and output factors. Input factors refer to the demand for emergency services. These can include demographic factors, or an increase in non-urgent visits to the ED due to multiple reasons.
Throughput factors refer to the processes within the ED, such as triage, diagnosis, and treatment. Inefficiencies in these processes can contribute to crowding. For instance, delays in diagnostic testing can result in longer patient stays in the ED.
Output factors refer to the transition of patients from the ED to other areas of the hospital or their discharge. For example, delays in hospital bed availability can result in ‘boarding’, where patients remain in the ED even after they are ready for admission, contributing to ED crowding

Strategies to Reduce ED Crowding
Every hospital and emergency room (ER) is distinctly different, and what works in one may not be a perfect fit for another. It’s crucial to recognize that strategies aren’t one-size-fits-all and can’t be copied. It’s highly recommended for each ER to conduct its improvement workshop, delving into the unique factors contributing to ED crowding and devising tailored improvement actions. Check out the article “How to Conduct the Kaizen Event” for guidance.
Before settling on solutions for ED crowding, a cross-functional team must collaborate to construct a Current State Value Stream Map. This detailed mapping of patient flow helps pinpoint bottlenecks. While this process isn’t straightforward, organizing a Kaizen Event is essential. Once the Current State VSM is complete and bottlenecks are identified, the team can transition to crafting a Future State VSM, paving the way for targeted and effective solutions.
Addressing ED crowding requires a comprehensive, system-wide strategy that transcends departmental boundaries.
However below is a list of strategies that have been implemented by various hospitals to address the problem of ED crowding.
- Simplification of Admission Process: Streamlining admissions reduces administrative delays, ensuring faster patient access to necessary care and freeing up ED resources promptly.
- Flow Management: Optimizing patient flow prevents bottlenecks, allowing for smoother transitions between departments, and reducing congestion in the ED.
- Efficient Transfer of Patients within the Hospital: Swift transfers to appropriate units ensure timely treatment continuation, preventing ED overcrowding by facilitating faster patient movement.
- Reducing Non-value Add Tasks Performed by Caregivers: Eliminating unnecessary tasks allows caregivers to focus on direct patient care, enhancing efficiency and reducing delays in the ED.
- Redirecting Non-emergent Cases to OPD: Directing less critical cases to OPD reserves ED resources for more urgent cases, minimizing unnecessary congestion.
- Better Internal Communication: Improved communication enhances coordination, leading to quicker decision-making, better patient management, and reduced ED wait times.
- Early Hospital Discharge: Facilitating timely discharges ensures ED beds are freed up promptly, contributing to efficient patient flow.
- Standard Clinical Pathways: Standardized treatment protocols reduce variability, streamline care processes, and enhance overall efficiency in the ED.
- Provider in Triage: Having a provider in triage accelerates initial evaluations, facilitating quicker decision-making and expediting patient care.
- Fast Track Area: A designated area for less severe cases allows for more efficient resource allocation, reducing ED congestion.
- Changing Staffing Pattern: Adjusting staffing levels based on demand ensures optimal resource utilization during peak times, preventing delays.
- Patient Flow Team: A dedicated team managing patient flow enhances coordination and ensures a smoother patient journey, reducing ED overcrowding.
- Housekeeping SWAT Teams: Rapid response teams for cleaning expedite bed turnover, minimizing wait times and improving ED efficiency.
- IP Bed Management Team: A team focused on inpatient bed availability facilitates quicker admissions, preventing ED overcrowding.
- Nursing Pool: Flexible nursing resources during high demand ensure sufficient staffing to manage increased patient volume, reducing delays in the ED.
- Quick Registration: Streamlining patient registration reduces administrative delays, contributing to faster patient care in the ED.
- Improved Diagnostic Turnaround: Enhancing diagnostic testing efficiency shortens ED stays by providing timely results, improving overall patient flow.
- High Probability Potential Admissions: Identifying high probability admissions allows proactive bed management, streamlining the admission process and reducing ED congestion.
Role of Technology in Managing ED Crowding
Technology plays a crucial role in managing ER crowding. Electronic health records can facilitate patient tracking, streamline communication, and improve patient flow. They can provide real-time data on wait times, bed availability, and patient status, enabling better resource allocation and decision-making.
Moreover, telemedicine can help alleviate ED crowding by providing remote consultation for non-urgent cases. This can reduce the demand for in-person ER visits, freeing up resources for more critical cases. Furthermore, predictive analytics can help forecast patient demand and resource needs, enabling proactive management of ED.
Conclusion
Emergency Department Crowding is a complex issue that requires a comprehensive and multifaceted approach. By understanding its causes and implementing effective strategies, it is possible to reduce ER waiting times, improve patient care, and enhance the overall functioning of the emergency department.